When it comes to compounded preparations, healthcare providers and patients alike want assurance that every treatment remains safe, effective, and reliable—from the first dose to the last. One of the most important factors in delivering that confidence is understanding how long a medication remains stable—and how those timeframes are determined.
That’s where stability testing and Beyond-Use Dates (BUDs) come in.
What Are Stability Studies?
A stability study is a scientific evaluation of how long a medication maintains its potency, sterility, and safety under defined storage conditions. According to the FDA, stability testing determines “how the quality of a drug substance or product varies with time under the influence of environmental factors such as temperature, humidity, and light, and establishes a retest period for the drug substance.”[1].
In practice, these studies subject medications to various controlled conditions and test for:
- Potency: Ensures the medication maintains its labeled strength.
- Sterility: Confirms the absence of microbial contamination[2].
- Endotoxin Levels: Checks for harmful byproducts.
The results of these tests help determine how long a compounded product remains both chemically stable and microbiologically safe—which defines its BUD[3].
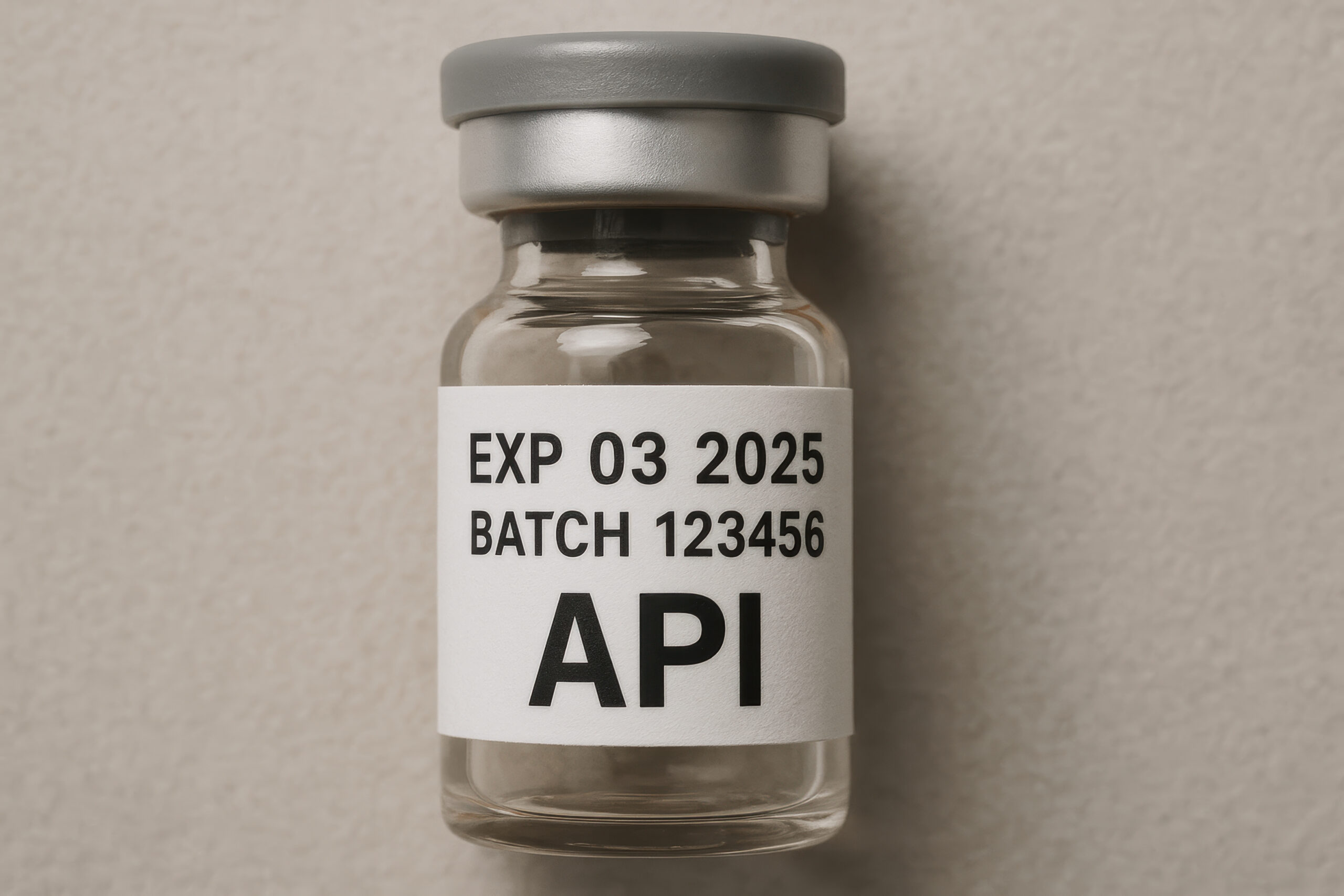
Expiration Dates vs. BUDs
In ProRx Pharma’s 503B compounding environment, expiration dates apply to raw materials—the active pharmaceutical ingredients (APIs) and excipients sourced from FDA-registered manufacturers. Each ingredient arrives with a Certificate of Analysis (CoA) and a manufacturer-assigned expiration date. That date reflects validated stability data and marks the period during which the ingredient is guaranteed to meet its labeled quality standards before compounding.
Once an ingredient is compounded into a finished, sterile preparation, the manufacturer’s expiration date no longer applies. From that point forward, a new, data-driven BUD governs the finished product’s lifecycle.
BUDs for Finished ProRx Products
After compounding, filtration, testing, and packaging within ISO-classified cleanrooms, ProRx assigns a BUD to every finished product. This date reflects validated evidence of how long that specific formulation remains stable, potent, and sterile under labeled storage conditions[4].
ProRx determines its BUDs through:
- Independent, third-party stability testing on key formulations[5].
- Sterility and endotoxin testing under cGMP controls[6].
- Container-closure integrity validation which confirms that each vial, syringe, or seal system maintains a sterile barrier and prevents contamination or leakage for the full duration of the product’s labeled BUD[7].
- Continuous environmental and quality monitoring across cleanroom operations[8].
Because ProRx invests in this level of validation, we can offer products that are potent, safe, and sterile that follow Code of Federal Regulations (CFR) and Current Good Manufacturing Practice (cGMP) guidelines—helping our healthcare partners:
- Reduce waste;
- Maintain steady inventory; and
- Ensure product reliability.
Why Stability Testing and BUD Validation Matter
Without stability testing, compounded drugs are subject to conservative U. S. Pharmacopeia (USP) default BUDs—sometimes only days or weeks[9]. By performing validated stability studies, ProRx extends product life safely and scientifically[10].
Importantly, for FDA-registered 503B outsourcing facilities like ProRx, stability testing isn’t just best practice—it’s a regulatory requirement. Under the Drug Quality and Security Act (DQSA) and FDA’s cGMP standards, 503Bs must perform validated stability studies to justify the BUDs printed on product labels[11]. This ensures that every ProRx medication maintains its potency, purity, and sterility throughout its labeled BUD—meeting both scientific and FDA compliance expectations.
Benefits for healthcare providers and patients include:
- Safety: Assurance that every compounded batch remains sterile and effective through its labeled BUD.
- Efficiency: Fewer reorders and less waste.
- Confidence: Products backed by independent validation and full FDA compliance.
Basically, an expiration date reflects the standard from the manufacturer. A BUD is for compounded medications based on scientific formula.
Independent Third-Party Testing: A ProRx Advantage
While all FDA-registered 503B outsourcing facilities are required to perform stability and sterility testing under cGMP standards[12], not all go the extra step of using independent, third-party laboratories.
At ProRx, we view external validation as a core element of scientific integrity. Our partnership with accredited, independent labs ensures that every stability and sterility test is conducted using validated, stability-indicating methods[13]—with objective results that confirm potency, purity, and sterility through the full BUD.
This additional layer of verification provides:
- Credibility: Independent documentation that meets or exceeds FDA expectations[14].
- Transparency: Clear, traceable data for healthcare providers and regulators.
- Confidence: Assurance that every batch we produce performs exactly as labeled, with no compromise in quality or safety.
By investing in third-party testing, ProRx goes beyond compliance—setting a higher standard for trust, accountability, and pharmaceutical precision in the 503B outsourcing industry.
Examples of ProRx Products with Validated Extended BUDs
ProRx’s third-party testing and internal Quality Assurance (QA) validation support extended BUDs for several in-demand therapies:
- Tirzepatide – 12 months
- Semaglutide – 12 months
- NAD⁺ (Nicotinamide Adenine Dinucleotide) – 146 days
- Sermorelin – 150 days
These extended BUDs reflect verified stability and sterility data, ensuring that every batch maintains its potency and purity for the full labeled period.
The ProRx Difference
Not every compounding pharmacy invests in full stability and sterility validation—but at ProRx Pharma, it’s foundational to our mission. By combining rigorous third-party testing with cGMP operations and quality-assurance oversight[15], we deliver compounded sterile and non-sterile preparations that meet the highest standards of safety, stability, and performance.
[1] FDA, 2003, Q1A(R2) Stability Testing of New Drug Substances and Products.
[2] 21 CFR 211.113, Control of Microbiological Contamination.
[3] USP, 2021, Compounding Standards (USP <795>, <797>).
[4] FDA, 2018, Current Good Manufacturing Practice – Guidance for Human Drug Compounding Outsourcing Facilities Under Section 503B of the FD&C Act; and 21 CFR 211.166, Stability testing.
[5] ProPharma Group, 2023, Stability Testing of New Drug Substances and Products.
[6] 21 CFR 211.113, Control of Microbiological Contamination.
[7] 21 CFR 211.94, Drug Product Containers and Closures; and USP, 2021, <1207> Package Integrity Evaluation – Sterile Products.
[8] USP, 2021, Compounding Standards (USP <797>).
[9] USP, 2021, Compounding Standards (USP <795>),
[10] FDA, 2003, Q1A(R2) Stability Testing of New Drug Substances and Products.
[11] FDA, 2018, Current Good Manufacturing Practice – Guidance for Human Drug Compounding Outsourcing Facilities Under Section 503B of the FD&C Act.
[12] 21 CFR 211.166, Stability Testing.
[13] Southwest Research Institute (SWRI), 2024. Stability Testing Studies.
[14] FDA, 2018, Current Good Manufacturing Practice – Guidance for Human Drug Compounding Outsourcing Facilities Under Section 503B of the FD&C Act.
[15] 21 CFR 211.166, Stability Testing; and FDA, 2018, Current Good Manufacturing Practice – Guidance for Human Drug Compounding Outsourcing Facilities Under Section 503B of the FD&C Act.